Perks policy for doctors challenged
Physician organization wants limits rolled back
By Liz Kowalczyk,
Boston Globe July 23, 2009
A growing number of hospitals, universities, and states are barring drug companies from buying physicians dinner, hiring them as speakers, and giving them even token gifts.
Now, a new organization of doctors - several from Boston - wants to roll back policies curbing interactions between doctors and drug company representatives, saying restrictive rules ultimately will hurt the patients they’re designed to protect.
The group, called the Association of Clinical Researchers and Educators, plans to hold its first conference today at Brigham and Women’s Hospital to promote “productive collaboration’’ between industry and physicians, which they say leads to better medicines and treatments. Dr. Jeffrey Flier, dean of Harvard Medical School, is one of 25 speakers and will give the welcoming remarks to about 200 attendees.
Flier, who is unaffiliated with the organization, will not endorse its views, said David Cameron, spokesman for the medical school, which is revising its conflict-of-interest policy. “He will welcome vigorous debate and analysis on the issue of academic collaborations with industry and encourage individuals with varied perspectives to participate in the discussion,’’ Cameron said in a written statement.
Dr. Thomas Stossel, an oncologist at the Brigham; Dr. Jeffrey Garber, chief of endocrinology at Harvard Vanguard Medical Associates; and Dr. Paul Richardson, an oncologist at Dana-Farber Cancer Institute, are among the founders of the group. Stossel said they want “to convey that there is a silent majority out there. And to restore some balance to the debate,’’ he said.
The group’s website says its long-term goals include reversing restrictive new conflict-of-interest policies and establishing chapters at universities and within medical specialty societies.
Massachusetts public health officials plan in two years to review the state’s new conflict-of-interest regulations, which went into effect July 1 and include a ban on gifts to doctors from drug and medical device companies, and Stossel said his group “wants to create an outcry against’’ the law. The law also requires drug and device companies to disclose publicly most payments made to doctors for consulting.
Partners HealthCare, which includes the Brigham and Massachusetts General Hospital, passed its own restrictions in April, which go further than the state law, banning all industry-paid gifts and meals and also forbidding doctors from traveling the country as paid members of company “speakers bureaus.’’
The association’s goals, which run contrary to the widespread movement in medicine to create more distance between doctors and pharmaceutical companies, have been widely discussed - and often derided - on healthcare blogs in the past several weeks.
Patient advocacy groups and lawmakers leading the charge for more restrictive policies say Stossel and his colleagues are misguided. Advocates of the restrictions believe drug companies, by giving doctors gifts and paying them to speak and consult, create bias in favor of their products, causing doctors to write more prescriptions for expensive new drugs even if patients don’t really need the medication or if an older, less expensive drug would work just as well.
Dr. Peter Slavin, president of Mass. General, has said that company-funded meals, gifts, and other practices don’t promote a positive image of doctors and increase healthcare costs.
“The rules benefit consumers by removing the conflicts that we know cloud judgment, and let doctors make decisions free from market pressures,’’ said Brian Rosman, research director for Health Care For All, a Boston-based patient advocacy group.
But Stossel and his colleagues said the new rules stifle invention. They believe the impact of small gifts and meals on doctors is negligible compared with the benefit of collaboration.
“I’ve been in medicine 40 years, and medicine is incomparably better than when I started out,’’ Stossel said. “I don’t think anyone can challenge the fact that it’s because of the tools we’ve gotten from industry.’’
Stossel is a former member of Cambridge-based Biogen Idec’s scientific advisory board. He said he now does occasional consulting to companies on conflict-of-interest policies. The conference is funded by attendees’ fees, though participants who work for drug and device companies are charged more, he said.
Sunday, July 26, 2009
Thursday, July 16, 2009
Schwarzenegger Replaces Most of State Nursing Board
by Tracy Weber - July 13, 2009 9:55 pm EDT
Tags: Arnold Schwarzenegger, California, California Board of Registered Nursing, Nurses
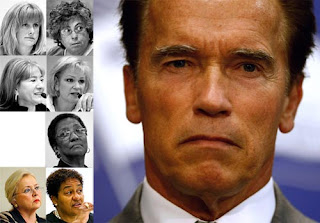
California Gov. Arnold Schwarzenegger (John Moore/Getty Images)California Gov. Arnold Schwarzenegger replaced nearly everyone on the Board of Registered Nursing late Monday, citing the unacceptable length of time it takes to discipline nurses accused of egregious misconduct.
Correction (July 14, 2009): This story incorrectly referred to former Board of Registered Nursing vice president Elizabeth O. Dietz as a professor of nursing at San Jose State. Although the board’s web site lists that as her current affiliation, the university said she retired in July 2008.
Update (July 14, 2009): Nursing Board Executive Officer Ruth Ann Terry Resigns [1]
Gov. Arnold Schwarzenegger replaced most members of the California Board of Registered Nursing on Monday, citing the unacceptable time it takes to discipline nurses accused of egregious misconduct.
He fired three of six sitting board members [2] – including President Susanne Phillips [3] – in two-paragraph letters curtly thanking them for their service. Another member resigned Sunday. Late Monday, the governor's administration released a list of replacements.
The shake-up came a day after the Los Angeles Times and ProPublica published an investigation [4] finding that it takes the board, which oversees 350,000 licensees, an average of three years and five months [5] to investigate and close complaints against nurses.
During that time, nurses accused of wrongdoing are free to practice – often with spotless records – and move from hospital to hospital. Potential employers are unaware of the risks, and patients have been harmed as a result.
Reporters found nurses who continued to work unrestricted for years despite documented histories of incompetence, violence, criminal convictions and drug theft or abuse. In dozens of cases, nurses maintained clean records in California even though they had been suspended or fired by employers, disciplined by another California licensing board or restricted from practice by other states.
"It is absolutely unacceptable that it takes years to investigate such outrageous allegations of misconduct against licensed health professionals whom the public rely on for their health and well-being," Schwarzenegger said in a written statement.
Board member Andrea Guillen Dutton, in a resignation letter Sunday [6], said she was leaving in frustration. "Certain ‘bad actors' are jeopardizing the reputation of the entire nursing profession," she wrote. "This deeply saddens me."
"I have fought to defend the integrity of patient care throughout the state by holding the negligent accountable," she wrote. "However, I have grown increasingly frustrated by the board's lack of ability to achieve its stated objectives in a timely and efficient manner."
Besides Phillips, the other fired board members were vice president Elizabeth O. Dietz, a former professor of nursing at San Jose State, and Janice Glaab, a public affairs consultant.
Schwarzenegger's action Monday fills two of three vacancies on the board [2] and replaces four of the board's sitting members – all of whom had been appointed by him.
The two remaining members are Nancy L. Beecham, appointed by the governor in 2006, and Dian Harrison, who was appointed last year by Assembly speaker Karen Bass.
Neither Beecham nor Harrison could be reached late Monday, nor could any of the departing board members.
Schwarzenegger's statement said his "administration is dedicated to protecting public health and safety, and the new board will act quickly and decisively to achieve that goal."
Fred Aguiar, secretary of the State and Consumer Services Agency, said in an interview that the new board would be asked immediately to come up with a plan to eliminate the case backlog. "This plan needs to include how many more investigators are needed, how much that will cost. … I want to know now."
California Board of Registered Nursing executive officer
 Ruth Ann Terry (Liz O. Baylen/Los Angeles Times)
Ruth Ann Terry (Liz O. Baylen/Los Angeles Times)
The governor's decision does not directly affect the standing of Ruth Ann Terry, who has been the board's executive officer for nearly 16 years and a staff member for 25. Only the board has the power to hire and fire the executive.
Terry, reached late Monday, hung up on a reporter, saying, "We don't have anything to say."
But Aguiar suggested Monday that Terry and other staffers could be vulnerable. The governor "supports the new board in its commitment to protecting patients – and if that means cleaning house, including board staff, so be it," he said. "The days of excuses and status quo are over. It's broken and we're going to fix it."
The Times and ProPublica
In an interview last week, Terry acknowledged that the system needed to be "streamlined" but blamed other parts of the state's bureaucracy for delays.
Early Monday, Terry and her assistant executive officer, Heidi Goodman,
"Ruth and I are aware of the grim picture painted by this article," they wrote, "however, the board members, managers and supervisors know that you work very hard to carry out the mission of the board to protect the healthcare consumers in California and we appreciate all that you do."
Presented with the investigation's findings Thursday, board President Phillips, a family nurse practitioner and associate clinical professor at UC Irvine, said she supported Terry "absolutely – without question."
"The issue of patient safety is of the utmost importance to this board," she said. "It's not that we are ignoring a situation where there are delays. We absolutely are not."
Questions about the board's leadership were first raised last fall
In addition to the governor's action, the state Senate Business and Professions Committee, which has jurisdiction over the board, plans to hold a hearing next month to address the issues raised in The Times' article.
The committee will look at introducing legislation that would appoint an "enforcement monitor" to evaluate the board's discipline process and make recommendations, said Bill Gage, the committee's chief consultant. Such a monitor was appointed at one time to work with the Medical Board of California, which regulates the state's doctors.
Consumer advocate Ken McEldowney said the board members need to do more than just fill seats.
"The leadership is key," said McEldowney, executive director of Consumer Action, a San Francisco-based national consumer advocacy and education membership organization.
"It just appears to me that they don't care."
The six new board members are: Ann Boynton, 47, of Sacramento, a former undersecretary for the Health and Human Services Agency; Judy Corless, 58, of Corona, a clinical nursing director at the Corona Outpatient Surgical
Center since April 2009; Jeannine Graves, 49, of Sacramento, a staff nurse for the Capitol Surgical Associates and the Mercy San Juan Medical Center; Richard Rice, 60, of Imperial Beach, a former chairman of the Unemployment Insurance Appeals Board; Catherine Todero, 57, of La Mesa, director of the school of nursing at San Diego State University and a professor there; and Kathrine Ware, 50, of Davis, a nurse practitioner for the Vascular Center Clinic at the University of California Davis.
These positions do not require Senate confirmation, and the compensation is $100 per working day.
[8] when The Times and ProPublica reported that nurses with serious or multiple criminal convictions kept their licenses for years before the board acted against them. As a result, the board now requires every nurse to submit fingerprints [9], which can be matched against arrest records. Renewing nurses must also disclose any convictions or discipline by other states.sent an e-mail to all board staff members encouraging them not to lose heart [7].found that the board relied heavily on Terry and her staff [4]. At five public meetings attended by reporters since November 2007, Terry never focused on the delays in disciplining errant nurses. Neither did board members, even though they must vet all disciplinary actions.
by Tracy Weber - July 13, 2009 9:55 pm EDT
Tags: Arnold Schwarzenegger, California, California Board of Registered Nursing, Nurses
California Gov. Arnold Schwarzenegger (John Moore/Getty Images)California Gov. Arnold Schwarzenegger replaced nearly everyone on the Board of Registered Nursing late Monday, citing the unacceptable length of time it takes to discipline nurses accused of egregious misconduct.
Correction (July 14, 2009): This story incorrectly referred to former Board of Registered Nursing vice president Elizabeth O. Dietz as a professor of nursing at San Jose State. Although the board’s web site lists that as her current affiliation, the university said she retired in July 2008.
Update (July 14, 2009): Nursing Board Executive Officer Ruth Ann Terry Resigns [1]
Gov. Arnold Schwarzenegger replaced most members of the California Board of Registered Nursing on Monday, citing the unacceptable time it takes to discipline nurses accused of egregious misconduct.
He fired three of six sitting board members [2] – including President Susanne Phillips [3] – in two-paragraph letters curtly thanking them for their service. Another member resigned Sunday. Late Monday, the governor's administration released a list of replacements.
The shake-up came a day after the Los Angeles Times and ProPublica published an investigation [4] finding that it takes the board, which oversees 350,000 licensees, an average of three years and five months [5] to investigate and close complaints against nurses.
During that time, nurses accused of wrongdoing are free to practice – often with spotless records – and move from hospital to hospital. Potential employers are unaware of the risks, and patients have been harmed as a result.
Reporters found nurses who continued to work unrestricted for years despite documented histories of incompetence, violence, criminal convictions and drug theft or abuse. In dozens of cases, nurses maintained clean records in California even though they had been suspended or fired by employers, disciplined by another California licensing board or restricted from practice by other states.
"It is absolutely unacceptable that it takes years to investigate such outrageous allegations of misconduct against licensed health professionals whom the public rely on for their health and well-being," Schwarzenegger said in a written statement.
Board member Andrea Guillen Dutton, in a resignation letter Sunday [6], said she was leaving in frustration. "Certain ‘bad actors' are jeopardizing the reputation of the entire nursing profession," she wrote. "This deeply saddens me."
"I have fought to defend the integrity of patient care throughout the state by holding the negligent accountable," she wrote. "However, I have grown increasingly frustrated by the board's lack of ability to achieve its stated objectives in a timely and efficient manner."
Besides Phillips, the other fired board members were vice president Elizabeth O. Dietz, a former professor of nursing at San Jose State, and Janice Glaab, a public affairs consultant.
Schwarzenegger's action Monday fills two of three vacancies on the board [2] and replaces four of the board's sitting members – all of whom had been appointed by him.
The two remaining members are Nancy L. Beecham, appointed by the governor in 2006, and Dian Harrison, who was appointed last year by Assembly speaker Karen Bass.
Neither Beecham nor Harrison could be reached late Monday, nor could any of the departing board members.
Schwarzenegger's statement said his "administration is dedicated to protecting public health and safety, and the new board will act quickly and decisively to achieve that goal."
Fred Aguiar, secretary of the State and Consumer Services Agency, said in an interview that the new board would be asked immediately to come up with a plan to eliminate the case backlog. "This plan needs to include how many more investigators are needed, how much that will cost. … I want to know now."
California Board of Registered Nursing executive officer
 Ruth Ann Terry (Liz O. Baylen/Los Angeles Times)
Ruth Ann Terry (Liz O. Baylen/Los Angeles Times)The governor's decision does not directly affect the standing of Ruth Ann Terry, who has been the board's executive officer for nearly 16 years and a staff member for 25. Only the board has the power to hire and fire the executive.
Terry, reached late Monday, hung up on a reporter, saying, "We don't have anything to say."
But Aguiar suggested Monday that Terry and other staffers could be vulnerable. The governor "supports the new board in its commitment to protecting patients – and if that means cleaning house, including board staff, so be it," he said. "The days of excuses and status quo are over. It's broken and we're going to fix it."
The Times and ProPublica
In an interview last week, Terry acknowledged that the system needed to be "streamlined" but blamed other parts of the state's bureaucracy for delays.
Early Monday, Terry and her assistant executive officer, Heidi Goodman,
"Ruth and I are aware of the grim picture painted by this article," they wrote, "however, the board members, managers and supervisors know that you work very hard to carry out the mission of the board to protect the healthcare consumers in California and we appreciate all that you do."
Presented with the investigation's findings Thursday, board President Phillips, a family nurse practitioner and associate clinical professor at UC Irvine, said she supported Terry "absolutely – without question."
"The issue of patient safety is of the utmost importance to this board," she said. "It's not that we are ignoring a situation where there are delays. We absolutely are not."
Questions about the board's leadership were first raised last fall
In addition to the governor's action, the state Senate Business and Professions Committee, which has jurisdiction over the board, plans to hold a hearing next month to address the issues raised in The Times' article.
The committee will look at introducing legislation that would appoint an "enforcement monitor" to evaluate the board's discipline process and make recommendations, said Bill Gage, the committee's chief consultant. Such a monitor was appointed at one time to work with the Medical Board of California, which regulates the state's doctors.
Consumer advocate Ken McEldowney said the board members need to do more than just fill seats.
"The leadership is key," said McEldowney, executive director of Consumer Action, a San Francisco-based national consumer advocacy and education membership organization.
"It just appears to me that they don't care."
The six new board members are: Ann Boynton, 47, of Sacramento, a former undersecretary for the Health and Human Services Agency; Judy Corless, 58, of Corona, a clinical nursing director at the Corona Outpatient Surgical
Center since April 2009; Jeannine Graves, 49, of Sacramento, a staff nurse for the Capitol Surgical Associates and the Mercy San Juan Medical Center; Richard Rice, 60, of Imperial Beach, a former chairman of the Unemployment Insurance Appeals Board; Catherine Todero, 57, of La Mesa, director of the school of nursing at San Diego State University and a professor there; and Kathrine Ware, 50, of Davis, a nurse practitioner for the Vascular Center Clinic at the University of California Davis.
These positions do not require Senate confirmation, and the compensation is $100 per working day.
[8] when The Times and ProPublica reported that nurses with serious or multiple criminal convictions kept their licenses for years before the board acted against them. As a result, the board now requires every nurse to submit fingerprints [9], which can be matched against arrest records. Renewing nurses must also disclose any convictions or discipline by other states.sent an e-mail to all board staff members encouraging them not to lose heart [7].found that the board relied heavily on Terry and her staff [4]. At five public meetings attended by reporters since November 2007, Terry never focused on the delays in disciplining errant nurses. Neither did board members, even though they must vet all disciplinary actions.
Saturday, July 4, 2009
Consumer Reports Profiles Survivor Alicia Cole
 Reform should make it easy to get information on quality
Reform should make it easy to get information on qualityAugust 2009
'I lay in my hospital bed watching my stomach turn black and purple and rot. It looked as if I had been snapped in half by a shark.'— Alicia Cole, 46, of Sherman Oaks, Calif.Photo by Melanie Eve Barocas
This article is the archived version of a report that appeared in the August 2009 Consumer Reports magazine.
When Alicia Cole learned she needed surgery for benign fibroids, she did her homework on the surgeon and the hospital. "I looked at HealthGrades, Leapfrog, Hospital Compare, and other Web sites," says Cole, a 46-year-old actress from Sherman Oaks, Calif. "But one thing I didn't check was the hospital's infection rate."
Even if she had tried to check, California hospitals didn't have to make such data public, and hers didn't. Cole had the operation there anyway. During her hospital stay, she came down with a post-surgical flesh-eating infection that turned her entire midsection into something worthy of a horror movie. After two months in the hospital and two years of painful rehabilitation, she still can't work. "The skin and scar tissue is so delicate that the least pressure will tear or scratch it," she says. Federal inspectors subsequently found unsterile conditions in the hospital's operating area.
Enraged by her experience, Cole joined the fight against hospital infections and helped persuade the California legislature to pass a law requiring public reporting; she now sits on the advisory board for the law. Did she ever learn the hospital's infection rate? Sadly, no. The law has not yet been implemented. "What we really need is a national law," Cole says, noting that hospital-acquired infections are a leading cause of death in this country. "It's the elephant in the room," she says.
CU recommends
Health reform should make it simple to get good information on health-care quality. You should be able to find data not only on infection rates, a reform we've backed for years, but also on doctors, drugs, treatments, and errors. Yet most states still allow doctors to shield a history of malpractice settlements. And infection rates, if reported at all, are often kept secret, which doesn't provide enough incentive for improvement.
What does work is disclosure. Pennsylvania, which passed the first statewide reporting law, remains the only state to require disclosure of all major types of hospital infections. And infections there have dropped 8 percent in the last two years.
Read about our latest reform efforts and our analysis of legislation as its being debated in Washington, D.C. in our Guide to Health-Care Reform.
Surgery Tech Suspected of Exposing 5,700 to Hepatitis C
Colorado Springs surgery tech suspected of exposing 5,700 to hepatitis C
July 2, 2009 - 6:28 PM
JOHN C. ENSSLIN AND BRIAN NEWSOME
THE GAZETTE
No vaccine for hepatitis C is available.
July 2, 2009 - 6:28 PM
JOHN C. ENSSLIN AND BRIAN NEWSOME
THE GAZETTE
Federal officials Thursday warned that about 5,700 surgery patients, including 1,000 at a Colorado Springs surgery center, are at risk of having been infected by an operating room technician with hepatitis C.
Colorado Springs surgery center, are at risk of having been infected by an operating room technician with hepatitis C.
 Colorado Springs surgery center, are at risk of having been infected by an operating room technician with hepatitis C.
Colorado Springs surgery center, are at risk of having been infected by an operating room technician with hepatitis C.On Thursday, federal authorities filed criminal charges in U.S. District Court in Denver against Kristen Diane Parker, a former scrub technician at Rose Medical Center in Denver and Audubon Ambulatory Surgery Center in Colorado Springs.
According to the criminal complaint, Parker - a former heroin addict - admitted swapping her own dirty syringes filled with saline solution for syringes filled with Fentanyl, a narcotic 80 to 100 times stronger than morphine.
The drug is supposed to be used to help major post-surgery patients manage pain. Instead, they got no relief while Parker injected herself with the painkiller at home and in the hospital bathrooms before and after a surgery, according to the seven-page complaint.
"I know I (expletive deleted) up," Parker told Denver Police Detective Dale Wallis after he confronted her during a videotaped interview on June 30. "I can't take back what I did, but I will have to live with it for the rest of my life, and so does everybody else."
She told Wallis she expects to spend the rest of her life in prison. She told the detective that she had used heroin from July 2008 to September 2008 while living in New Jersey. She said she had used dirty needles and "was 99.9 percent sure" that is how she was exposed to hepatitis C.
A MySpace page for a woman with the name Kristen Parker describes her as a 26-year-old Colorado Springs resident with interests in heavy metal rock, tattoos and needles.
"I have a crazy fascination with needles.. I just like the way they feel!" the Web page states.
According to an affidavit by Mary F. LaFrance, an investigator for the U.S. Food and Drug Administration, at least nine surgery patients at Rose have tested positive for the incurable disease.
As a result, authorities are advising 4,700 Rose patients and 1,000 Audubon patients that they may have been exposed and need to be tested.
Parker worked at Rose from October 21, 2008 until April 2009. She resigned on April 20 from Rose, but the hospital refused to accept her resignation and instead fired her.
She went to work for Audubon shortly after being fired from Rose. She worked there from May 4 until Monday, said Dr. J. Michael Hall, Audubon's medical director.
Hall said certified letters are being sent to all patients who had outpatient surgery at the center's Circle Drive and Union Boulevard location May 4-July 1 advising them they may have been exposed and with instructions on what to do. Patients at Audubon's two other locations, one near St. Francis Medical Center and a pain management center, are unaffected.
In the criminal complaint she is charged with tampering with a consumer product, creating a counterfeit controlled substance and obtaining a controlled substance "by deceit and subterfuge."
If convicted, she faces up to 10 years in prison and a maximum $250,000 on the most serious charge of tampering. She also faces state charges.
Parker is not a nurse and holds no medical degree although she is trained as a surgical technician. Her job involved preparing operating rooms prior to surgery.
Prior to being hired at Rose, she submitted to a pre-employment blood test which tested positive for hepatitis C. She was allowed to start work but hospital officials counseled her about the disease and exposure possibilities.
Rose placed her on administrative leave following an incident in which a co-worker was pricked by a needle in Parker's pocket on March 23, 2009.
According to the affidavit, Parker quickly disposed of the needle and denied any use of narcotics. She was allowed to return to work after a drug screening test came back negative.
The hospital placed her on administrative leave again after a co-worker reported seeing Parker in an operating room to which she was not assigned. She was tested again for drugs and this time the results were positive for Fentalyn.
The hospital had a press conference Thursday and released a prepared statement that apologized to patients who have been affected.
"It is impossible to adequately express how deeply sorry and angry we are that the unconscionable acts of this terminated employee may have put some of our patients at risk," the statement reads.
The hospital will offer free testing to surgery patients of the hospital or the outpatient surgery center. Also, hospital officials have created a phone line for affected patients and their families who have questions.
After an investigation by the Colorado Department of Health, Parker was ordered by the state to "immediately cease and desist any employment that requires contact with patients and/or pharmaceuticals."
Hall said his center learned of the situation Thursday from the Colorado Department of Public Health and Environment. State and local health authorities, as well as Atlanta physicians with the federal Centers for Disease Control and Prevention, are assisting in tracking the exposures.
Hepatitis C facts
Hepatitis C facts
According to the Centers for Disease Control Web site, about 15 to 25 percent of people infected with hepatitis C clear the virus and do not develop chronic infection for reasons that are not well known.
Those who do develop acute hepatitis C develop symptoms such as fever, fatigue, dark urine, abdominal pain, loss of appetite, clay colored stool, nausea, vomiting, joint pain and jaundice.
For every 100 people who contract the disease, 75 to 85 will develop a chronic infection. About 60 to 70 will develop chronic liver disease. About 5 to 20 will develop cirrhosis over a period of 20 to 30 years. Between 1 and 5 will die of liver cancer or cirrhosis.
Chronic hepatitis C infections account for about 8,000 to 10,000 deaths each year in the United States.
No vaccine for hepatitis C is available.
Subscribe to:
Posts (Atom)