By DENISE GRADY
By DENISE GRADY Efforts to make hospitals safer for patients are falling short, researchers report in the first large study in a decade to analyze harm from medical care and to track it over time.
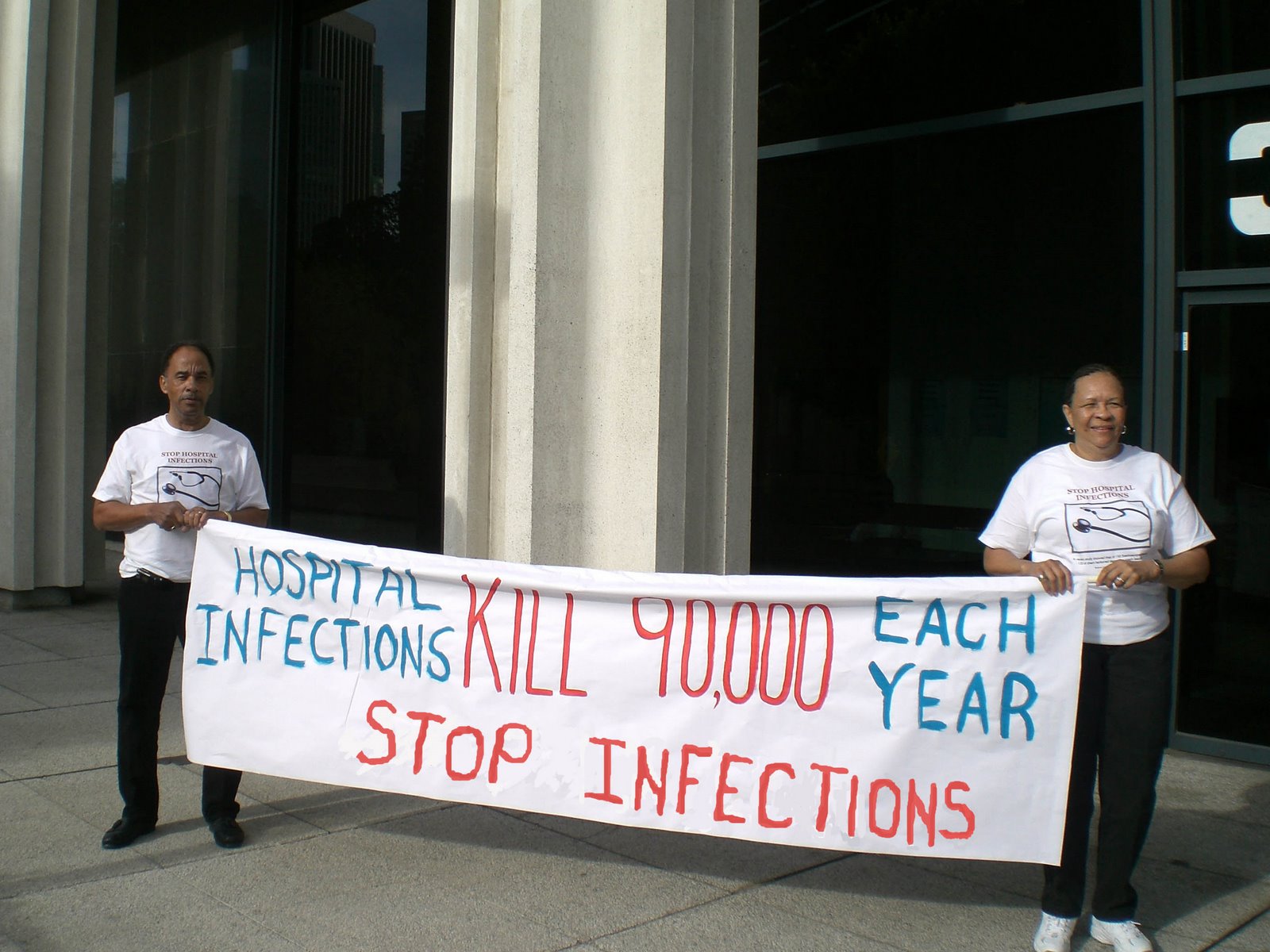
The study, conducted from 2002 to 2007 in 10 North Carolina hospitals, found that harm to patients was common and that the number of incidents did not decrease over time. The most common problems were complications from procedures or drugs and hospital-acquired infections.
“It is unlikely that other regions of the country have fared better,” said Dr. Christopher P. Landrigan, the lead author of the study and an assistant professor at Harvard Medical School. The study is being published on Thursday in The New England Journal of Medicine.
It is one of the most rigorous efforts to collect data about patient safety since a landmark report in 1999 found that medical mistakes caused as many as 98,000 deaths and more than one million injuries a year in the United States. That report, by the Institute of Medicine, an independent group that advises the government on health matters, led to a national movement to reduce errors and make hospital stays less hazardous to patients’ health.
Among the preventable problems that Dr. Landrigan’s team identified were severe bleeding during an operation, serious breathing trouble caused by a procedure that was performed incorrectly, a fall that dislocated a patient’s hip and damaged a nerve, and vaginal cuts caused by a vacuum device used to help deliver a baby.
Dr. Landrigan’s team focused on North Carolina because its hospitals, compared with those in most states, have been more involved in programs to improve patient safety.
But instead of improvements, the researchers found a high rate of problems. About 18 percent of patients were harmed by medical care, some more than once, and 63.1 percent of the injuries were judged to be preventable. Most of the problems were temporary and treatable, but some were serious, and a few — 2.4 percent — caused or contributed to a patient’s death, the study found.
The findings were a disappointment but not a surprise, Dr. Landrigan said. Many of the problems were caused by the hospitals’ failure to use measures that had been proved to avert mistakes and to prevent infections from devices like urinary catheters, ventilators and lines inserted into veins and arteries.
“Until there is a more coordinated effort to implement those strategies proven beneficial, I think that progress in patient safety will be very slow,” he said.
An expert on hospital safety who was not associated with the study said the findings were a warning for the patient-safety movement. “We need to do more, and to do it more quickly,” said the expert, Dr. Robert M. Wachter, the chief of hospital medicine at the University of California, San Francisco.
A recent government report found similar results, saying that in October 2008, 13.5 percent of Medicare beneficiaries — 134,000 patients — experienced “adverse events” during hospital stays. The report said the extra treatment required as a result of the injuries could cost Medicare several billion dollars a year. And in 1.5 percent of the patients — 15,000 in the month studied — medical mistakes contributed to their deaths. That report, issued this month by the inspector general of the Department of Health and Human Services, was based on a sample of Medicare records from patients discharged from hospitals.
Dr. Landrigan’s study reviewed the records of 2,341 patients admitted to 10 hospitals — in both urban and rural areas and involving large and small medical centers. (The hospitals were not named.) The researchers used a “trigger tool,” a list of 54 red flags that indicated something could have gone wrong. They included drugs used only to reverse an overdose, the presence of bedsores or the patient’s readmission to the hospital within 30 days.
The researchers found 588 instances in which a patient was harmed by medical care, or 25.1 injuries per 100 admissions.
Not all the problems were serious. Most were temporary and treatable, like a bout with severe low blood sugar from receiving too much insulin or a urinary infection caused by a catheter. But 42.7 percent of them required extra time in the hospital for treatment of problems like an infected surgical incision.
In 2.9 percent of the cases, patients suffered a permanent injury — brain damage from a stroke that could have been prevented after an operation, for example. A little more than 8 percent of the problems were life-threatening, like severe bleeding during surgery. And 2.4 percent of them caused or contributed to a patient’s death — like bleeding and organ failure after surgery.
Medication errors caused problems in 162 cases. Computerized systems for ordering drugs can cut such mistakes by up to 80 percent, Dr. Landrigan said. But only 17 percent of hospitals have such systems.
For the most part, the reporting of medical errors or harm to patients is voluntary, and that “vastly underestimates the frequency of errors and injuries that occur,” Dr. Landrigan said.
“We need a monitoring system that is mandatory,” he said. “There has to be some mechanism for federal-level reporting, where hospitals across the country are held to it.”
Dr. Mark R. Chassin, president of the Joint Commission, which accredits hospitals, cautioned that the study was limited by its list of “triggers.” If a hospital had performed a completely unnecessary operation, but had done it well, the study would not have uncovered it, he said. Similarly, he said, the study would not have found areas where many hospitals have made progress, such as in making sure that patients who had heart attacks or heart failure were sent home with the right medicines.
The bottom line, he said, “is that preventable complications are way too frequent in American health care, and “it’s not a problem we’re going to get rid of in six months or a year.”
Dr. Wachter said the study made clear the difficulty in improving patients’ safety.
“Process changes, like a new computer system or the use of a checklist, may help a bit,” he said, “but if they are not embedded in a system in which the providers are engaged in safety efforts, educated about how to identify safety hazards and fix them, and have a culture of strong communication and teamwork, progress may be painfully slow.”
Leah Binder, the chief executive officer of the Leapfrog Group, a patient safety organization whose members include large employers trying to improve health care, said it was essential that hospitals be more open about reporting problems.
“What we know works in a general sense is a competitive open market where consumers can compare providers and services,” she said. “Right now you ought to be able to know the infection rate of every hospital in your community.”
For hospitals with poor scores, there should be consequences, Ms. Binder said: “And the consequences need to be the feet of the American public.”