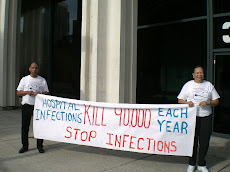
I really wish this Medicare ruling had included Hospital Acquired Infections (HAIs) such as in my case Necrotizing Fasciitis or Man-eating flesh disease. In a case where a patient is in above average health with no prexisting conditions and gets a nosocomial infection following a routine procedure, there should be no charge as well. My hospital made a fabulous profit from the two months I was fighting for my life in their facility.
MSN Money The Basics March 7, 2008
Hospitals won't get to bill for errors
As of October, Medicare will no longer cover treatment resulting from eight types of mistakes, and patients won't have to pay. States and private insurers are also pushing for change.
By Melinda Fulmer
Under pressure from large private insurers, state governments and Medicare, hospitals around the country are now agreeing not to charge when they make medical mistakes, also called "never events" because they shouldn't happen.
Though it may sound like a no-brainer not to charge patients who had surgery on the wrong body part or were disabled from the wrong medication, in the hospital world it is a revolution.
"Asking hospitals to commit to normal customer-service principles should not be radical, but it is," said Rachel Weissburg of The Leapfrog Group, a nonprofit organization that pushed for the move. "We have a very strange system in the U.S., where you don't pay for quality, you pay for service."
That's beginning to change, experts say. Starting in October, Medicare, which covers 44 million elderly and disabled people, won't pay for treatment resulting from eight types of hospital errors, including surgical objects left in a patient during surgery, patient falls, catheter-caused urinary-tract infections and pressure sores, the most common preventable medical error.
Nor will hospitals be able to bill injured patients for these conditions. So a patient who in the course of treatment for a heart attack incurred pressure sores -- bedsores -- would be billed only for the cardiac treatment.
Next year, several more preventable errors will likely be added to the list, including drug-resistant staph infections and ventilator-associated pneumonia, a Medicare spokesperson said. The move is expected to save the government $190 million over five years.
The heat is on The movement to get hospitals to clean up their acts has been building since 2005, when pioneering insurance provider HealthPartners of Minnesota first said it would not pay for hospital errors, Weissburg said.
The next year, The Leapfrog Group took it a step further, pressing hospitals to tear up bills for medical mistakes, report them, apologize to the patients affected and launch investigations into their causes. So far, a little more than half of the 1,300 hospitals it surveys for quality and safety have agreed to this policy.
Under this kind of pressure, state hospital associations and the American Hospital Association are now urging their members to voluntarily agree not to charge for a list of 28 so-called never events published by the National Quality Forum.
Washington Gov. Christine Gregoire recently announced that three state medical groups, including the Washington State Hospital Association, had agreed not to charge for serious medical errors. That came on the heels of action in Vermont and Minnesota, Weissburg said.
This 13-inch-long surgical retractor was left in the body of Donald Church, of Lynnwood, Wash., by a University of Washington Medical Center surgeon during an operation to remove a tumor in June 2000.
Reinforcing these voluntary arrangements is a new resolve among the insurers and agencies that pay the bills. Medicare isn't the only one putting away the checkbook.
Pennsylvania's Department of Public Welfare said last month that it, too, would stop Medicaid payments for errors, following similar moves by Minnesota and Massachusetts. And large insurers such as Aetna, Blue Cross and Blue Shield are modifying contracts to make hospitals absorb the costs of their own mistakes.
"Fortunately, these events are quite rare," said Dr. Troyen Brennan, Aetna's chief medical officer. "However, it is important to take steps that will increase hospitals' focus on why never events happen, promote shared information and facilitate improved processes that will prevent future events."
There's no nationwide system for tallying medical errors. Only about half of the states require any kind of reporting of medical mistakes, Weissburg said.
In Washington state, for example, 193 never events were reported out of 630,000 admissions.
Mistakes must be acknowledged This move has been slow in coming, analysts say, because it forces hospitals to admit fault, a move that could aid malpractice lawsuits. Los Angeles tort attorney Peter K. Levine said that might be true.
"It's just one more arrow in our quiver," he said. But, he adds, with expert witnesses, serious mistakes generally aren't that difficult to prove in court. And, he said, it may cut down on the number of lawsuits, as more angry patients are mollified.
"Treating the customer right goes a long way to preventing litigation," Levine said.
But will withholding pay really improve care? Hospital groups say it will because it provides an incentive for people to point out imminent mistakes.
Under Washington State Hospital Association guidelines, many of the people in an operating room will not be paid if a mistake happens. So anesthesiologists, nurses and others have more reason to speak up if they see a physician about to make an error, said Cassie Sauer, a spokeswoman for the Washington association.
Of course, these hospital guidelines are voluntary, so there's no guarantee that everyone will follow them.
But, Weissburg said, with insurers, medical groups and Medicare turning up the pressure, hospitals have no choice but to improve their game. "The culture is changing -- it's being forced to change."
What Medicare won't pay for:
An object mistakenly left in a patient during surgery.
A preventable air embolism.
Complications from being given incompatible blood.
Catheter-associated urinary-tract infections.
Pressure ulcers (bedsores).
A vascular catheter-associated infection.
A surgery-site infection after coronary-artery-bypass graft surgery.
Patient falls.
Some hospitals won't charge for these never events:
Surgery on the wrong body part.
Surgery on the wrong patient.
The wrong surgical procedure.
Unintentionally leaving a foreign object inside a patient during surgery.
A postoperative death of a normal, healthy patient.
An infant discharged to the wrong person.
A patient suicide or attempted suicide resulting in serious disability.
A maternal death or serious disability in a low-risk pregnancy.
A death or serious disability (brain damage) associated with jaundice in infants.
Stage 3/4 pressure ulcers (bedsores).
Artificial insemination with the wrong donor sperm or wrong egg.
Any incident in which a line designated for oxygen or other gas to be delivered contains the
wrong gas or toxic substances.
Care ordered by someone impersonating a physician, a nurse, a pharmacist or other licensed health-care provider.
Abduction of a patient.
Sexual assault of a patient.
A death or significant injury of patient or staff from physical assault.
The same hospitals won't charge for a patient death or serious disability:
Caused by contaminated drugs, devices or biologics.
Linked to the use or function of a device other than as intended.
Associated with an intravascular air embolism.
Associated with a patient escaping or leaving without permission.
From a medication error.
Linked to a reaction to incompatible blood or blood products.
Associated with hypoglycemia.
Due to spinal manipulative therapy.
Associated with electric shock.
Associated with a burn incurred while hospitalized.
Associated with a fall.
Linked to the use of restraints.
Subscribe to:
Post Comments (Atom)







No comments:
Post a Comment