Emma Hitt, PhD
March 23, 2010 (Atlanta, Georgia) — Hospital-onset healthcare-facility-associated Clostridium difficile infections (CDI) have increased in incidence and have surpassed methicillin-resistant Staphylococcus aureus (MRSA) infections, according to a new study of a large cohort of patients from community hospitals.
Becky A. Miller, MD, an infectious disease fellow from Duke University in Durham, North Carolina, presented the findings during an oral session here at the Fifth Decennial International Conference on Healthcare-Associated Infections 2010.
"This is the first time this has been described using patient-level data (i.e., with the number of cases as the numerator and the number of patient days as the denominator)," Dr. Miller told Medscape Infectious Diseases.
"We think this trend, particularly in community hospitals, would not have been captured without our large network of 39 hospitals where we perform infection control and surveillance," she said. "We were also unaware that cases of nosocomial C difficile infection had increased and surpassed MRSA."
The researchers performed a prospective cohort study in 28 community hospitals participating in the Duke Infection Control Outreach Network between January 2008 and December 2009.
The cohort consisted of 3,007,457 patient-days. Numerically, nosocomial CDI was the most common healthcare-associated infection (847 cases), followed closely by nosocomial bloodstream infection (838 cases).
Nosocomial infections due to MRSA and intensive care unit device-related infections were approximately equal, at 680 and 681 cases, respectively.
Patients with nosocomial CDI (n = 840) and nosocomial MRSA (n = 655) were equally likely to be male, and to have diabetes or end-stage renal disease requiring hemodialysis. However, patients who developed nosocomial CDI were, on average, older than patients who developed nosocomial MRSA infection (65 vs 59 years; P < .0001). In addition, time to infection was, on average, 8 days for CDI and 7 days for MRSA infection (P < .0001), and overall mortality was higher among patients with MRSA infection than CDI (P < .0001).
The rate of nosocomial CDI was 0.28 cases per 1000 patient-days, whereas the rate of nosocomial MRSA infection was 0.23 cases per 1000 patient-days. Thus, nosocomial CDI occurred 25% more frequently than nosocomial MRSA infection.
Since 2007, rates of healthcare-associated MRSA infection have steadily decreased, whereas rates of CDI have increased, Dr. Miller said during her presentation.
According to Dr. Miller, C difficile spores are shed in stool, and these spores can persist in the hospital environment for months. "These infections are not being prevented by methods that are clearly working to prevent nosocomial infections due to MRSA," she said. She added that "we think that this study represents the tip of the iceberg, as we did not include nosocomial C difficile cases diagnosed after patients leave the hospital."
In another presentation on C difficile, researchers described a targeted strategy to eliminate C difficile using ultragermicidal bleach wipes. Robert Orenstein, DO, from the Mayo Clinic in Rochester, Minnesota, reported the findings here in a poster session.
"The beauty of this project was that implementation was relatively simple — it required putting together a committed team and emphasizing our goal of improving patient outcomes," Dr. Orenstein told Medscape Infectious Diseases.
The researchers targeted 2 units with a focused intervention of daily cleaning of all patient rooms with Clorox brand ultragermicidal bleach wipes containing 6.15% sodium hypochlorite, and cleaning after the patient had been discharged.
Cleaning was assessed by environmental services supervisors, and Clean-Trace technology was used. Patients and environmental services employees who cleaned the rooms responded to a survey regarding satisfaction and tolerance of the cleaning procedure.
Before the intervention was initiated, the incidence of CDI was 18.4 per 10,000 patient-days; after the intervention was initiated, the incidence was 3.76 per 10,000 patient-days, "far exceeding" their goal of a reduction in incidence of 30%, Dr. Orenstein said.
According to the authors, patients tolerated the cleaning well, and although environmental services "employees initially had concerns regarding odor and irritation, these were resolved." The cost of the intervention was estimated at $18,671 per year.
"I am struck by the fact that our highest-risk unit has gone 6 months without a hospital-acquired case attributable to their unit, despite the fact that the overall incidence (i.e., cases admitted with this infection) continues to rise," Dr. Orenstein said. "This suggests what we did really had a great impact," he added. "This is especially gratifying knowing the impact that C difficile disease can have on our patients lives."
"C difficile has been in the news for the last decade," said Carlene A. Muto, MD, medical director for infection control at the University of Pittsburgh School of Medicine in Pennsylvania. "What has taken focus this year is that the environment matters," she said.
According to Dr. Muto, an analysis by their group presented in the late-breaking session described the undetected reservoir in patients who asymptomatically carry C difficile (~6% of the patients tested).
"Many studies have described noncompliance with cleaning patient rooms and how a focused effort can change this behavior," Dr. Muto told Medscape Infectious Disease. "Our group implemented a bleach/detergent cleaning program years ago, but since June 2009, we have used this product on every surface, every time, not just in the rooms of patients known to be positive."
She noted that "patients not known to be colonized/infected one day may be so the next. We did see a decrease in C difficile healthcare-associated infections using this approach."
Neither study was commercially funded. Dr. Miller, Dr. Orenstein, and Dr. Muto have disclosed no relevant financial relationships.
Fifth Decennial International Conference on Healthcare-Associated Infections (ICHAI) 2010: Abstract 386, presented March 20, 2010; Abstract 142, presented March 19, 2010.
Showing posts with label HAI. Show all posts
Showing posts with label HAI. Show all posts
Sunday, April 11, 2010
Tuesday, November 10, 2009
Sebelius Announces Release of Recovery Act Funding to Improve Care in Nation’s Ambulatory Surgical Centers
To reduce healthcare-associated infections (HAIs) in stand-alone or same-day surgical centers, the HHS Secretary Kathleen Sebelius today announced the availability of up to $9 million in funding from the American Recovery and Reinvestment Act (ARRA) to state survey agencies in 43 states. HAIs are infections some patients acquire when they are in a health care setting such as a hospital or outpatient clinic.
“Because of the Recovery Act, millions of patients who go to stand-alone surgical centers will have greater assurance that they won’t come home with a new infection,” said Health and Human Services’ Secretary Kathleen Sebelius. “Residents in these 43 states will continue to see the benefits from the Recovery Act not only by addressing health care associated infections, but by putting people to work to solve an important issue and improve the quality of life for Americans.”
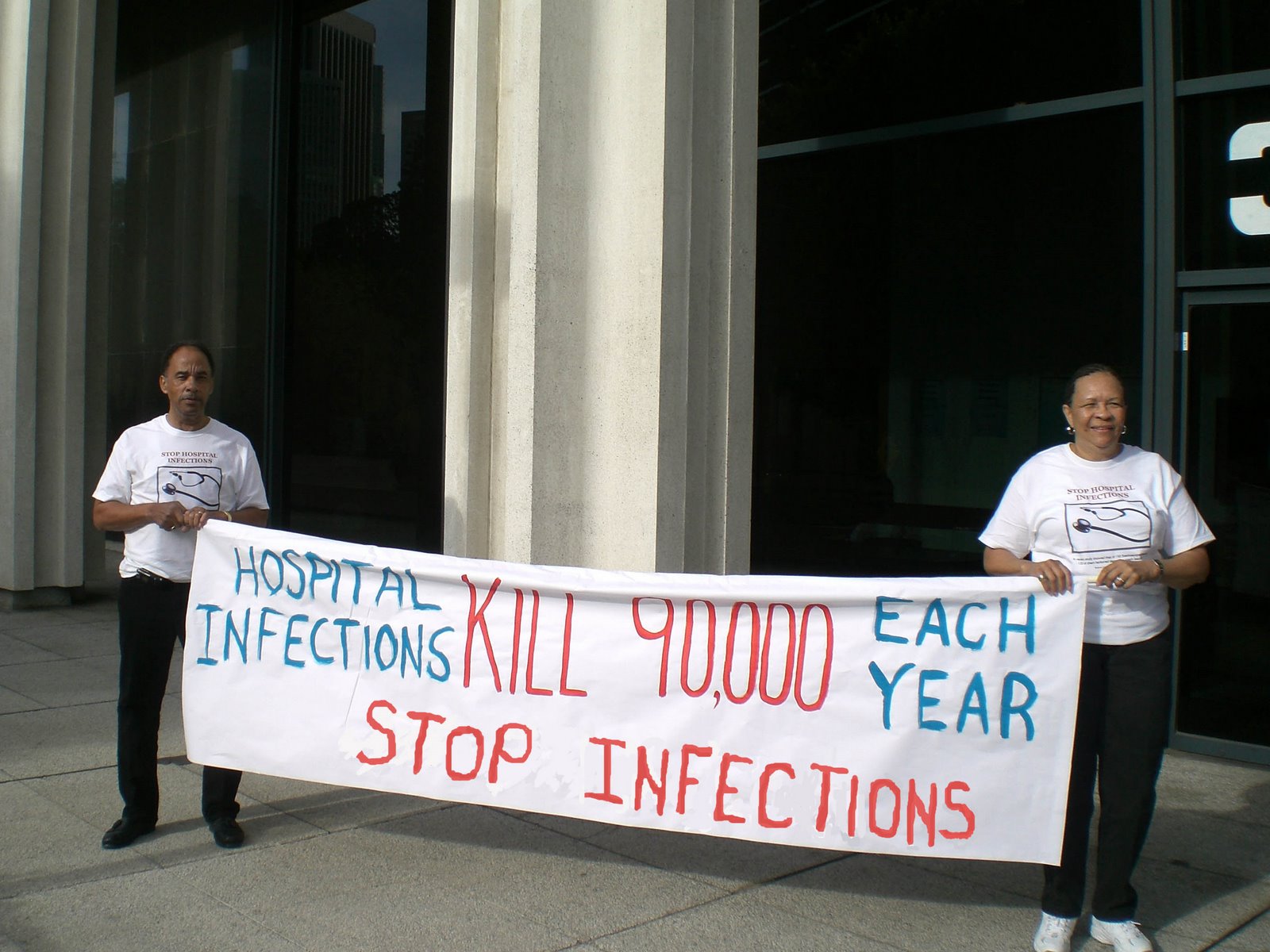
“Healthcare-Associated Infections kill nearly 100,000 people and add an extra $30 billion in healthcare costs every year. But with a little bit of knowledge, and some extra effort, much of that can be prevented. I’m glad to see these funds going to help put people to work combating this tragedy around the country,” said Congressman Dave Obey (D-WI), the Chairman of the House Appropriations Committee, who was a lead author of the Recovery Act and has been an outspoken advocate for efforts to reduce HAIs.
Accredited facilities are surveyed by CMS-approved private accrediting organizations. As part of the new initiative, surveyors in the 43 states will survey approximately 1,300 ambulatory surgical centers (ASCs) across the nation, one-third of the more than 3,800 non-accredited ASCs across the country during the next 12 months. State surveyors will employ a new CMS survey process for ASCs that uses an infection control tool developed in conjunction with the Centers for Disease Control and Prevention (CDC).
Across the United States, health care services are being shifted to outpatient settings such as ambulatory care facilities, long term care facilities, and free-standing specialty care sites. The number of ASCs participating in Medicare grew from about 3600 in calendar year 2002 to 5200 in early 2009, a 44 percent increase. ASCs account for more than 43 percent of all same-day (ambulatory) surgery in the United States, amounting to about 15 million procedures every year. Typical surgical procedures conducted in ASCs include endoscopies and colonoscopies, orthopedic procedures, plastic/reconstructive surgeries, and eye, foot, and ear/nose/throat surgeries.
HAI outbreaks in outpatient settings continue to occur according to the CDC. In several ASC-related communicable disease outbreaks, failure to employ very basic infection control practices were implicated, leading CMS to identify this as an area for additional oversight.
In the last fiscal year, 12 states volunteered to get a head start on this nationwide effort to reduce healthcare-associated infections in stand-alone or same-day surgical centers by beginning to survey ASCs with funding of nearly $1 million provided through the Recovery Act.
In addition to the funds being made available for the inspection of ASCs, the CDC has also made $40 million available to state public health departments to create or expand state-based HAI prevention and surveillance efforts, and strengthen the public health workforce trained to prevent HAIs.
These funds support activities outlined in HHS’ 2009 Action Plan to Prevent Healthcare-Associated Infections. The plan also establishes national goals, prioritizes recommended clinical practices, and coordinates a national research agenda. Development of this national plan, available at http://www.hhs.gov/ophs/initiatives/hai, is coordinated by HHS’ Office of Public Health and Science, and involves participation from the Agency for Healthcare Research and Quality, CDC, CMS, the Food and Drug Administration, the Indian Health Service, the Health Resources and Services Administration, the National Institutes of Health, the Office of the National Coordinator for Health Information Technology, and other HHS offices, and the Department of Veterans Affairs.
“Because of the Recovery Act, millions of patients who go to stand-alone surgical centers will have greater assurance that they won’t come home with a new infection,” said Health and Human Services’ Secretary Kathleen Sebelius. “Residents in these 43 states will continue to see the benefits from the Recovery Act not only by addressing health care associated infections, but by putting people to work to solve an important issue and improve the quality of life for Americans.”
“Healthcare-Associated Infections kill nearly 100,000 people and add an extra $30 billion in healthcare costs every year. But with a little bit of knowledge, and some extra effort, much of that can be prevented. I’m glad to see these funds going to help put people to work combating this tragedy around the country,” said Congressman Dave Obey (D-WI), the Chairman of the House Appropriations Committee, who was a lead author of the Recovery Act and has been an outspoken advocate for efforts to reduce HAIs.
Accredited facilities are surveyed by CMS-approved private accrediting organizations. As part of the new initiative, surveyors in the 43 states will survey approximately 1,300 ambulatory surgical centers (ASCs) across the nation, one-third of the more than 3,800 non-accredited ASCs across the country during the next 12 months. State surveyors will employ a new CMS survey process for ASCs that uses an infection control tool developed in conjunction with the Centers for Disease Control and Prevention (CDC).
Across the United States, health care services are being shifted to outpatient settings such as ambulatory care facilities, long term care facilities, and free-standing specialty care sites. The number of ASCs participating in Medicare grew from about 3600 in calendar year 2002 to 5200 in early 2009, a 44 percent increase. ASCs account for more than 43 percent of all same-day (ambulatory) surgery in the United States, amounting to about 15 million procedures every year. Typical surgical procedures conducted in ASCs include endoscopies and colonoscopies, orthopedic procedures, plastic/reconstructive surgeries, and eye, foot, and ear/nose/throat surgeries.
HAI outbreaks in outpatient settings continue to occur according to the CDC. In several ASC-related communicable disease outbreaks, failure to employ very basic infection control practices were implicated, leading CMS to identify this as an area for additional oversight.
In the last fiscal year, 12 states volunteered to get a head start on this nationwide effort to reduce healthcare-associated infections in stand-alone or same-day surgical centers by beginning to survey ASCs with funding of nearly $1 million provided through the Recovery Act.
In addition to the funds being made available for the inspection of ASCs, the CDC has also made $40 million available to state public health departments to create or expand state-based HAI prevention and surveillance efforts, and strengthen the public health workforce trained to prevent HAIs.
These funds support activities outlined in HHS’ 2009 Action Plan to Prevent Healthcare-Associated Infections. The plan also establishes national goals, prioritizes recommended clinical practices, and coordinates a national research agenda. Development of this national plan, available at http://www.hhs.gov/ophs/initiatives/hai, is coordinated by HHS’ Office of Public Health and Science, and involves participation from the Agency for Healthcare Research and Quality, CDC, CMS, the Food and Drug Administration, the Indian Health Service, the Health Resources and Services Administration, the National Institutes of Health, the Office of the National Coordinator for Health Information Technology, and other HHS offices, and the Department of Veterans Affairs.
Subscribe to:
Posts (Atom)