Gathering Highlights Growth of National Nurses Movement
More than 1,000 registered nurses from across the country rallied in Washington DC Wednesday, raising an unprecedented, unified voice for patient safety reforms and new, national standards for patient care conditions and standards for nurses.
The event was sponsored by the nation’s largest nurses’ union and professional association, the 155,000-member National Nurses United, which came to Washington to press the case for quality of care legislation that was not part of the national healthcare bill enacted earlier this year, and to build on the unity of RNs who are NNU members from coast to coast.
In addition to a march, rally, and conference, the RNs visited nearly 100 members of Congress, prodding legislators to work on the unfinished business of healthcare reform, quality of care and patient safety. The actions coincided with National Nurses Week.
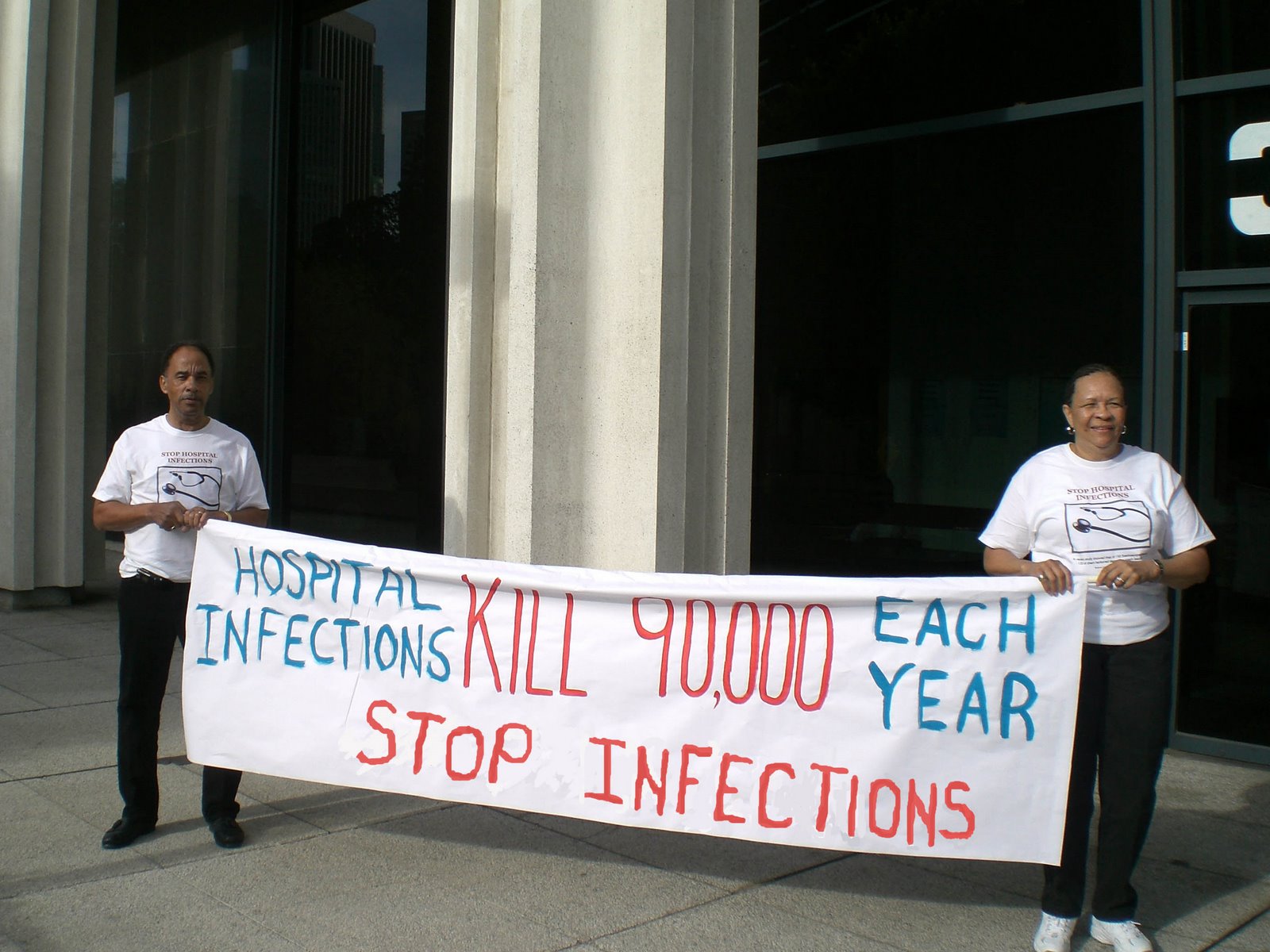
Noting recent national attention on the West Virginia mining disaster and the Gulf Coast oil spill, NNU Co-President Jean Ross, RN said that “similar accidents happen every day away from the media spotlight in U.S. hospitals and other healthcare settings. It’s time to act to protect our patients and our communities.”
"We're the voice of not only nurses but patients across the country,” said NNU Co-President Karen Higgins, RN. “When we leave this room I want everyone to remember that. When it comes time to make decisions about healthcare and people say 'leave it to the experts,' tell them 'I am the expert.' "
Among the legislative solutions are S 1031/HR 2133 that would, among other components, establish minimum ratios of nurses to patients for all U.S. hospitals, modeled after a successful California law, and S 1788/HR 2381 which would also promote nurse retention and reduce patient accidents and injuries by establishing safe patient lifting and handling policies.
Sen. Al Franken of Minnesota, author of S 1788, hosted a hearing on the bill Tuesday at which several nurses on hand for the week cited experiences that demonstrated the need for the bill.
Speaking Wednesday to an NNU rally across from the Capitol, Franken told the RNs, "You are the ones we look to for advice, comfort, expertise and care. You are tireless advocates for the country's well-being. You're the ones we trust to care for our loved ones, that's what your expertise is, and it's simply unacceptable that you're putting your own health on the line to care for patients."
"Now it's time to make sure that all nurses in all states have access to a safe workplace. One injured nurse is one too many. Employers have a fundamental obligation to put in place a safe working environment for all workers and nurses are no exception," Franken said.
Rep. Lynn Woolsey of California, speaking to the nurses, also emphasized why the bill is needed, "We don't need to create another patient in the process of caring for one."
U.S. Labor Secretary Hilda Solis, who also addressed the conference, told the nurses that more than 36,000 health care workers were injured by lifting and transferring patients, according to 2008 Bureau of Labor Statistics data. In addition, she said, 12 percent of nurses who plan to leave the profession cited back injuries as a contributing factor.
“What a waste when the career of an experienced nurse is ended years or decades too early because of an easily preventable back injury,” Solis said. “In these days of ever-rising health care costs, what a waste of money to pay workers compensation and disability for easily preventable back injuries.”
S 1031 author Sen. Barbara Boxer of California and HR 2133 author Rep. Jan Schakowsky of Illinois also spoke the NNU event about the ratio legislation which, according to a groundbreaking study from the University of Pennsylvania released last month, could have cut post-surgical patient deaths by 14 percent in New Jersey and 11 percent in Pennsylvania, two comparable states the researchers compared to California.
"We know that nurse-to-patient ratios work, and it is time to enact them around the nation. California was the testing ground and it's working," Boxer said. "Too often you are overworked because of staffing levels that are inadequate and that is unacceptable."
The Penn study, from noted researcher Linda Aiken, RN, PhD, documents “what California nurses have seen every day at the bedside since passage of the law -- safer care conditions, an enhanced quality of life for patients, and, as an added bonus, reduced burnout for nurses which mitigates the nursing shortage,” said California RN and NNU co-president Deborah Burger.
NNU is also seeking passage of HR 949/S 362 to restore equal collective bargaining rights for Veterans Affairs nurses.
Strengthening the rights of direct care RNs and their ability to more effectively advocate for patients and their colleagues, was another major theme of the NNU gathering.
"We've got to say something in a united way that tells employers it's a new day in America and RNs are going to stand up and not take it anymore," NNU Executive Director Rose Ann DeMoro said.
The RNs unanimously endorsed a resolution to establish national collective bargaining standards that notes the growing attack by many hospital employers against nurses and patient safety conditions.
The resolution notes that NNU will oppose “concessionary agreements that are injurious to our patients, our members, and our profession that undermine all represented RN contract standards” that include reductions in health coverage, pensions and other retirement security, two-tier programs for new hires, and reductions that impair patient safety.
Additionally, the resolution pledges NNU to fight for enhanced RN staffing and other improvements in patient care standards, improved retirement security for RNs, limits on the introduction of new technology that displaces RNs or RN professional judgment, and additional workplace safety measures.